Studies of diabetes and weight-loss drugs are underway to determine if they could also help manage a range of other conditions such as polycystic ovary syndrome (PCOS) and alcohol abuse.
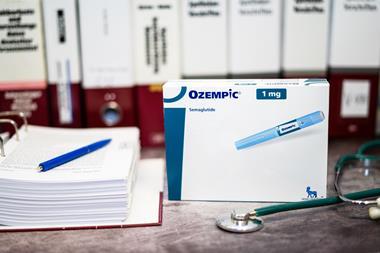
Semaglutide is the active substance in the branded Ozempic and Wegovy medications, which have been widely prescribed off-label for weight loss. Use of these drugs can see patients lose more than 10% of their body mass – but high demand has led to an Ozempic shortage in the UK. Researchers are now conducting clinical trials to see if semaglutide-based medications could also be beneficial in additional indications.
Novo Nordisk, the company that produces Wegovy, has suggested in late-stage trial results that injections of its drug could reduce the risk of major cardiovascular events – stroke or heart attack – by 20% in people who are overweight, or obese .
It has been estimated that Wegovy could prevent up to 1.5 million heart attacks over the next 10 years, according to a study published in Cardiovascular Drugs and Therapy, partly funded by Novo Nordisk.
Ozempic, which is also made by Novo Nordisk, is approved for lowering blood sugar levels in adults with type 2 diabetes (T2DM). According to the New York Times, a smaller trial found that the drug could also reduce the risk of heart complications in diabetes patients.
It is also hoped that semaglutide can improve symptoms of PCOS. The disorder – which can cause hormone imbalances and infertility – is linked to insulin resistance and a higher risk of T2DM. Weight loss can make improve some PCOS symptoms, according to the UK’s National Health Service (NHS).
Dr Harshal Deshmukh, a consultant endocrinologist and senior clinical lecturer at the University of Hull, Yorkshire is running a trial to explore the effect of semaglutide on weight, androgen reduction and quality of life in women with PCOS.
There are also plans to explore the impact of semaglutide on conditions not linked to excess weight, such as addiction disorders.
Ozempic and Wegovy mimic GLP-1, a hormone that promotes feelings of fullness, and seems to dampen the reward associated not only with food but also drugs. The idea came about after people given GLP-1 analogues for diabetes reported reductions in their alcohol consumption.
Dr Christian Hendershot, director of the clinical and translational addiction research programme at the University of North Carolina at Chapel Hill, USA, said: “We know that drugs in this class are remarkably effective for several important health outcomes – many of which can influence longevity and quality of life.”